What is the cause of such artifacts in cytogenetics
The phenomenon of artifacts in cytogenetic cultures and explore potential reasons for their occurrence
Cytogenetic Artifacts: Artifacts are unexpected or unintended changes or patterns observed during cytogenetic analysis
These artifacts can sometimes mimic true chromosomal abnormalities, leading to misinterpretation
Possible Causes of Artifacts:Sample Quality: Poor-quality samples (e.g., clotted bone marrow, degraded cells) can introduce artifacts. Contaminants or improper handling during sample collection can also play a role
Cell Culture Conditions: Variations in culture conditions (e.g., temperature, pH, nutrient availability) may affect cell growth and division, leading to artifacts
Cell Synchronization: Asynchronous cell populations (cells at different stages of the cell cycle) can introduce irregularities during metaphase spread preparation
Chromosome Spreading Techniques: Inadequate spreading of chromosomes on slides can result in overlapping or folded chromosomes, creating artifacts
Slide Preparation: Uneven distribution of cells on slides, improper fixation, or air-drying artifacts can occur during slide preparation
Staining Techniques: Inconsistent or improper staining methods may lead to artifacts
Chromosomal Mosaicism: Presence of cells with different chromosomal complements (e.g., trisomy, monosomy) can create mosaic patterns that resemble abnormalities.
Research and Investigation: Researchers and cytogeneticists continuously study these artifacts to improve diagnostic accuracy.
Identifying specific factors contributing to artifacts helps refine laboratory protocols and minimize their occurrence
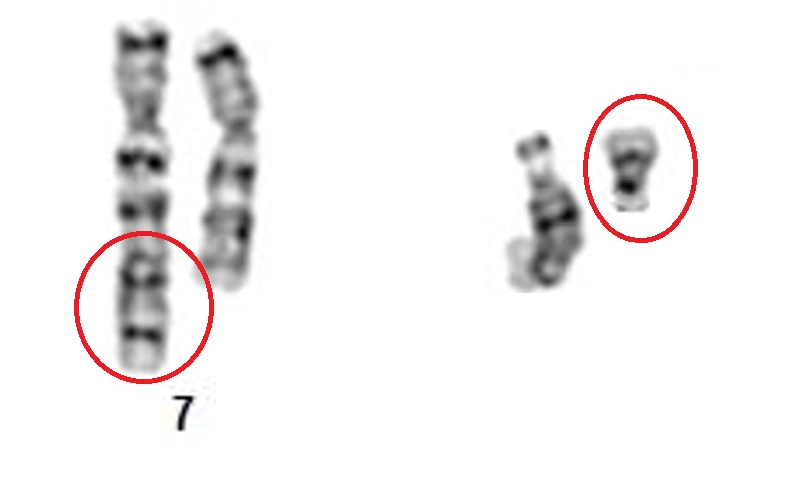
What is the cause of such artifacts in cytogenetics? t(7;14)
T-lymphocytes with 7;14 translocations: frequency of occurrence, breakpoints, and clinical and biological significance
G W Dewald, K J Noonan, J L Spurbeck, D D Johnson
- PMID: 3486591
- PMCID: PMC1684808
Abstract
Among 11,915 consecutive patients and 37 normal controls who had chromosome analysis at the Mayo Clinic between 1978 and 1984, 83 had a single sporadic metaphase with a 7;14 translocation. In 81 of the translocations, the breakpoints were at 14q11 and either 7q34 (type I) or 7p13 (type II): type I translocations occurred in 42 patients, and type II, in 39. The two other translocations had different breakpoints: one was t(7;14)(q11;q32), and the other was t(7;14)(p13;q32). All type I and type II translocations occurred in phytohemagglutinin-stimulated lymphocyte cultures; their combined incidence was 4.88 X 10(-4) per metaphase (81 of 165,991 metaphases) in such cultures. No type I or II translocation was found among 6,713 fibroblast metaphases, 33,463 amniocyte metaphases, or 68,972 bone marrow and unstimulated peripheral blood metaphases. One variant 7;14 translocation occurred in a phytohemagglutinin-stimulated culture, and the other occurred in a fibroblast culture. We did not find a correlation of sporadic 7;14 translocations with any month or season of the year or with patient age or sex. Of the 83 patients, 78 had various clinical disorders, three had ataxia-telangiectasia, one was a normal control, and one was an artificial insemination donor. Follow-up studies on 64 (77%) patients indicate that, to date, none have developed any malignant process subsequent to chromosome analysis. Except for ataxia-telangiectasia, the occurrence of types I and II translocations in lymphocyte cultures may have little, if any, clinical significance. The biological significance of these translocations may be the association of genes in chromosome bands 14q11, 7p13, and 7q34 with the normal physiology of lymphocytes such as the alpha- and beta-chains for T-cell antigen receptor.

دیدگاه خود را بنویسید